Targeting AR Signaling in Prostate Cancer
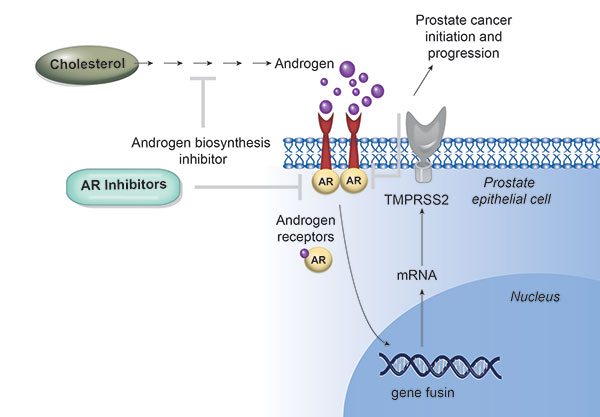
In prostate cancer, androgen steroid hormones bind to the androgen receptor (AR) and thereby trigger a key lineage-specific, oncogenic transcriptional program. Targeting the AR signaling axis has been, over decades, the mainstay of prostate cancer therapy. More potent inhibitors of androgen synthesis and antiandrogens have emerged and have been successfully implemented in clinical practice. Although androgen-deprivation therapies and/or the administration of first-generation competitive AR inhibitors prevent further tumor growth for a while, most patients develop resistance to the treatment and subsequently progress to castration-resistant prostate cancer (CRPC).
PARP Inhibitors in Prostate Cancer
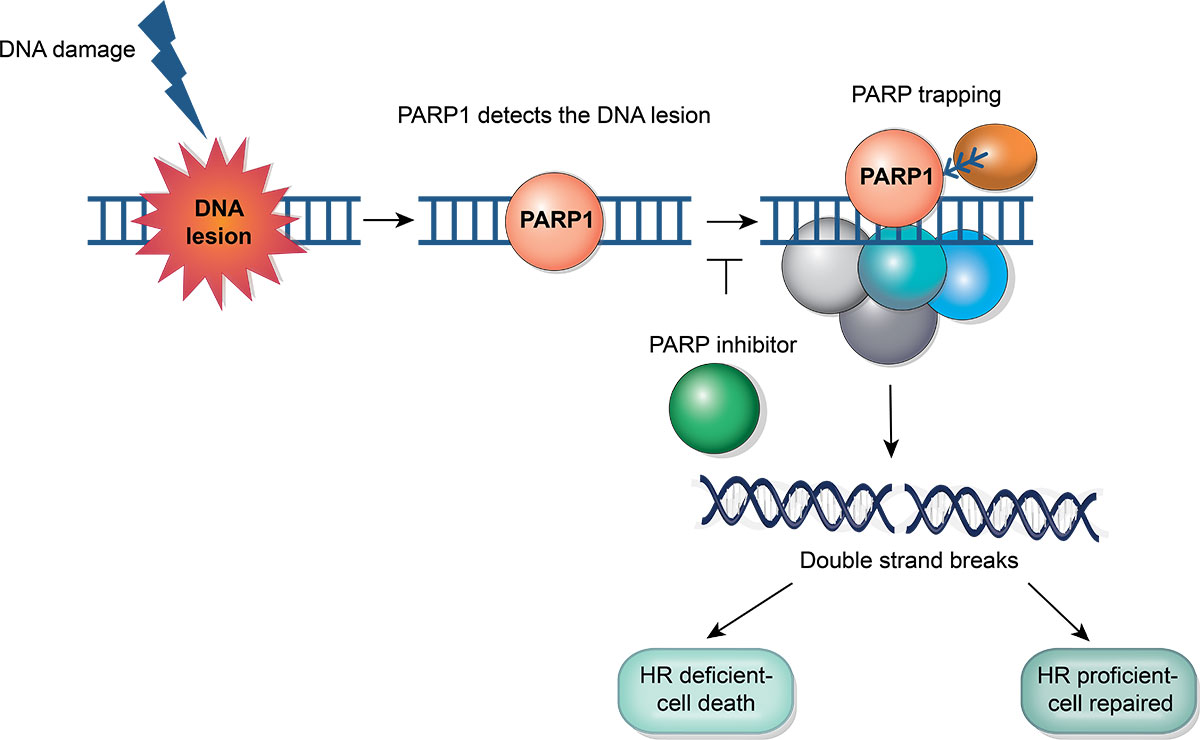
Poly-ADP ribose polymerase inhibitors (PARPi) represent a burgeoning treatment avenue in addressing prostate cancer. Their key mode of operation involves triggering synthetic lethality in cells that harbor deficiencies in homologous recombination repair (HRR). Clinical studies have demonstrated that in individuals with metastatic castrate-resistant prostate cancer (mCRPC) and specific alterations in the HRR pathway, PARPi treatment has been shown to induce objective tumor responses as well as improve progression free and overall survival.
Nuclear Imaging and Theranostics for Prostate Cancer
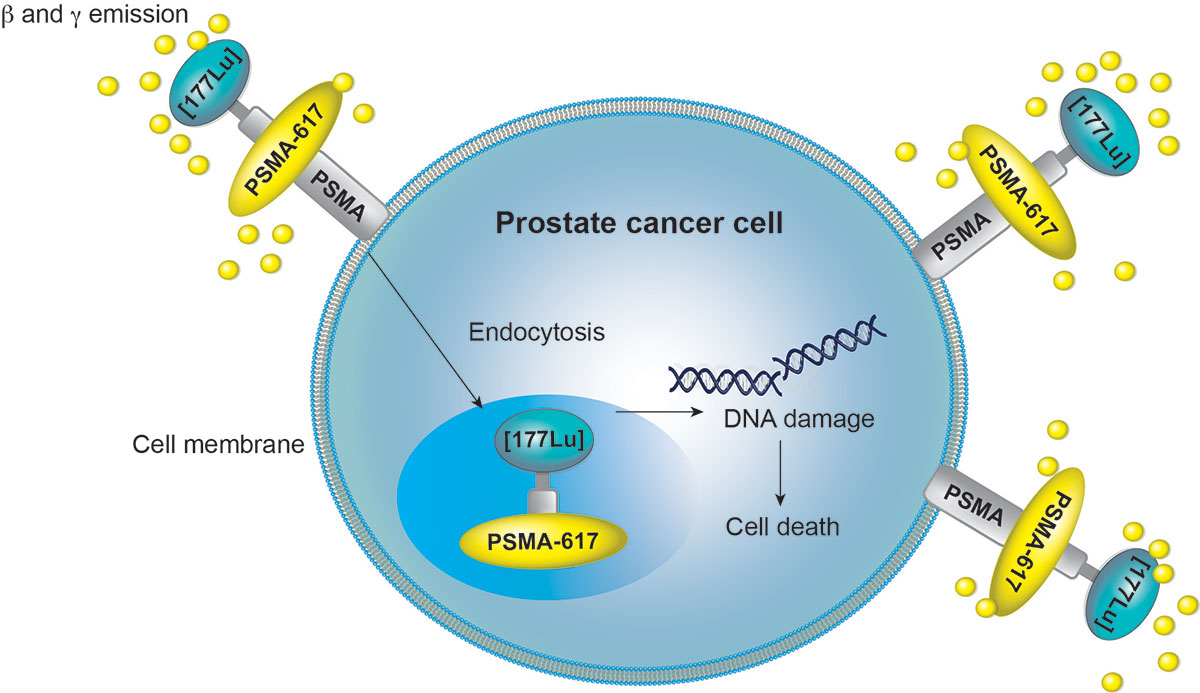
Prostate cancer ranks as the second most common epithelial neoplasm among men aged 50 and older, following skin cancer. Prostate-specific antigen (PSA) levels serve as an early screening tool for detection. Various radiological methods are employed for imaging prostate cancer, ranging from ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) to hybrid nuclear medicine techniques like single-photon emission computed tomography (SPECT)/CT and positron emission tomography (PET)/CT. Advancements in radiopharmaceutical compounds have introduced specific tracers with both diagnostic and therapeutic applications, significantly broadening the scope for targeted and highly effective clinical management of prostate cancer patients.
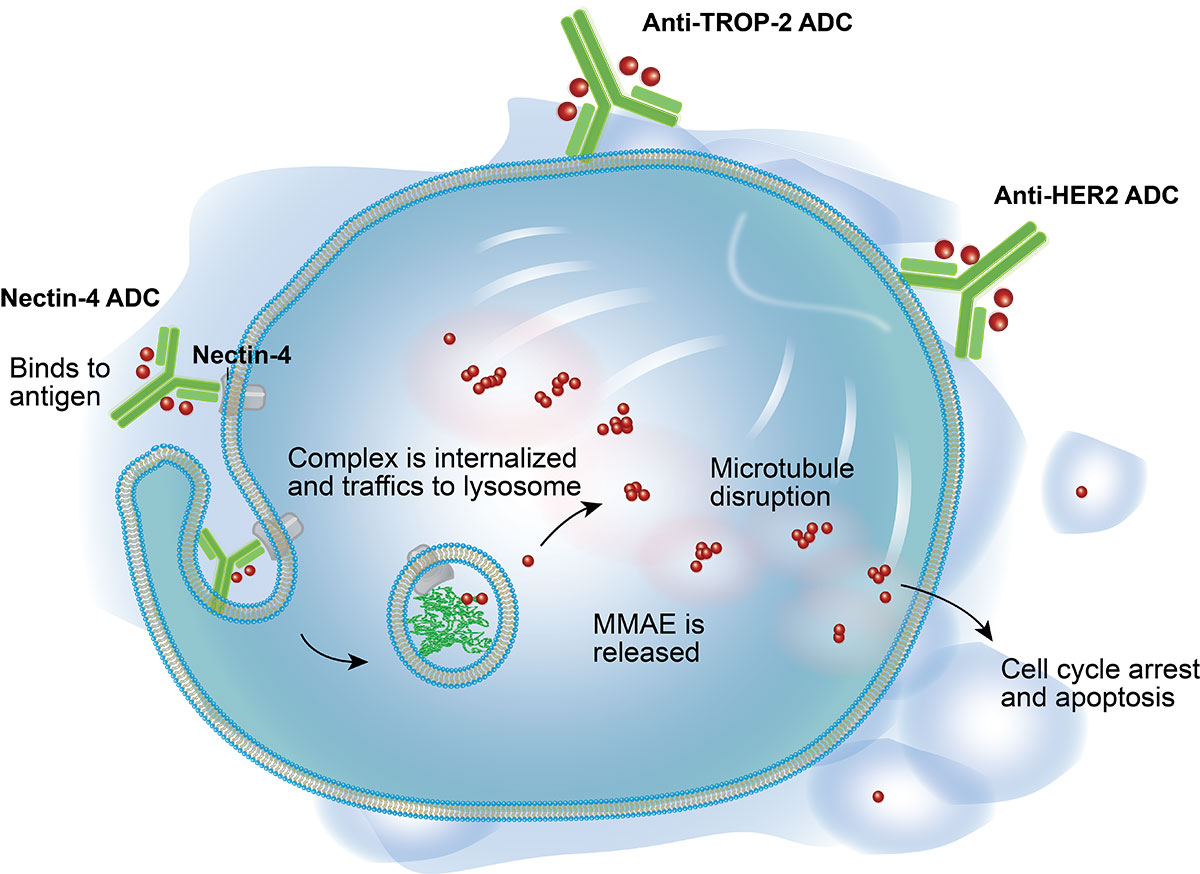
Antibody-Drug Conjugates in
Urothelial Carcinoma
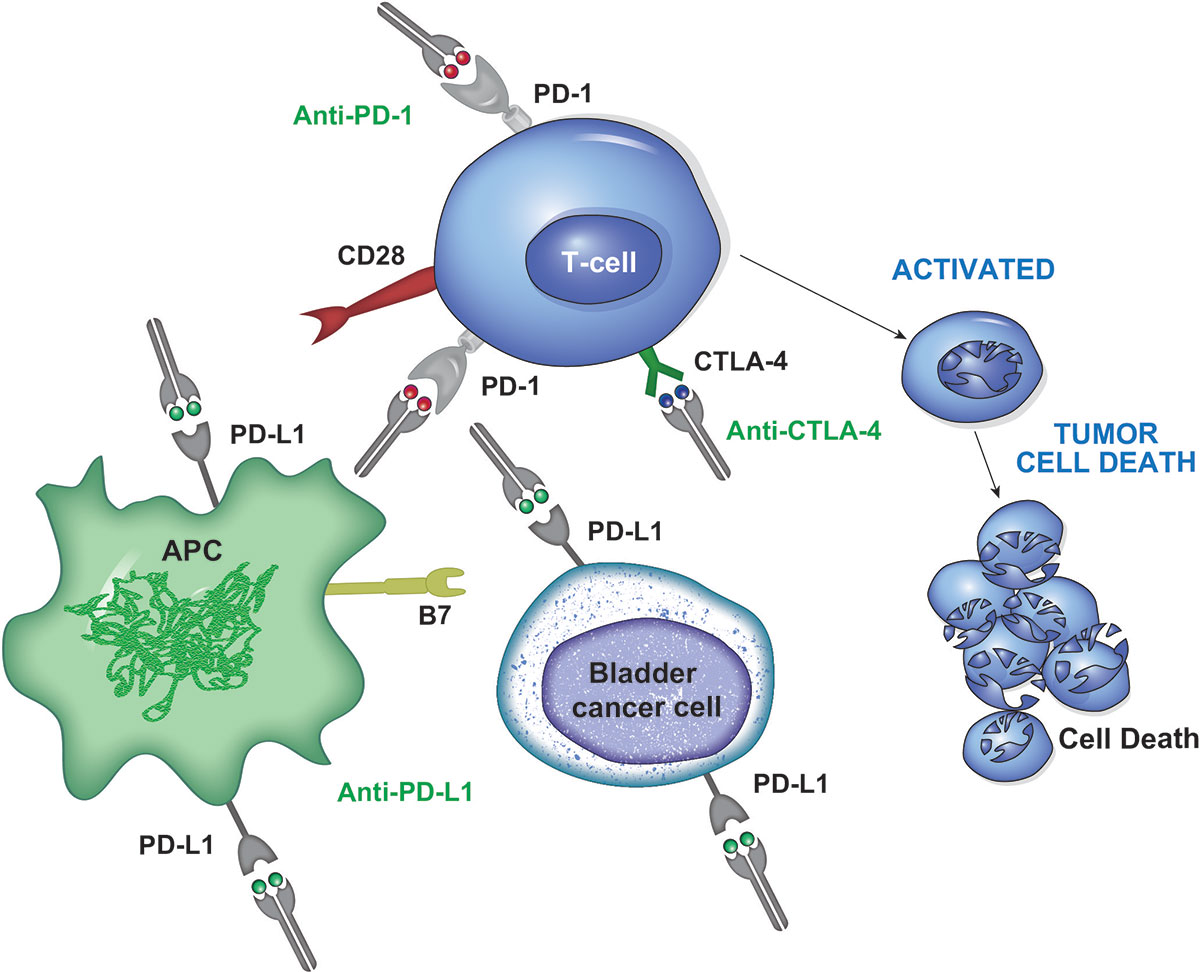
Checkpoint Inhibitors in
Urothelial Carcinoma
Targeting FGFR in
Urothelial Carcinoma
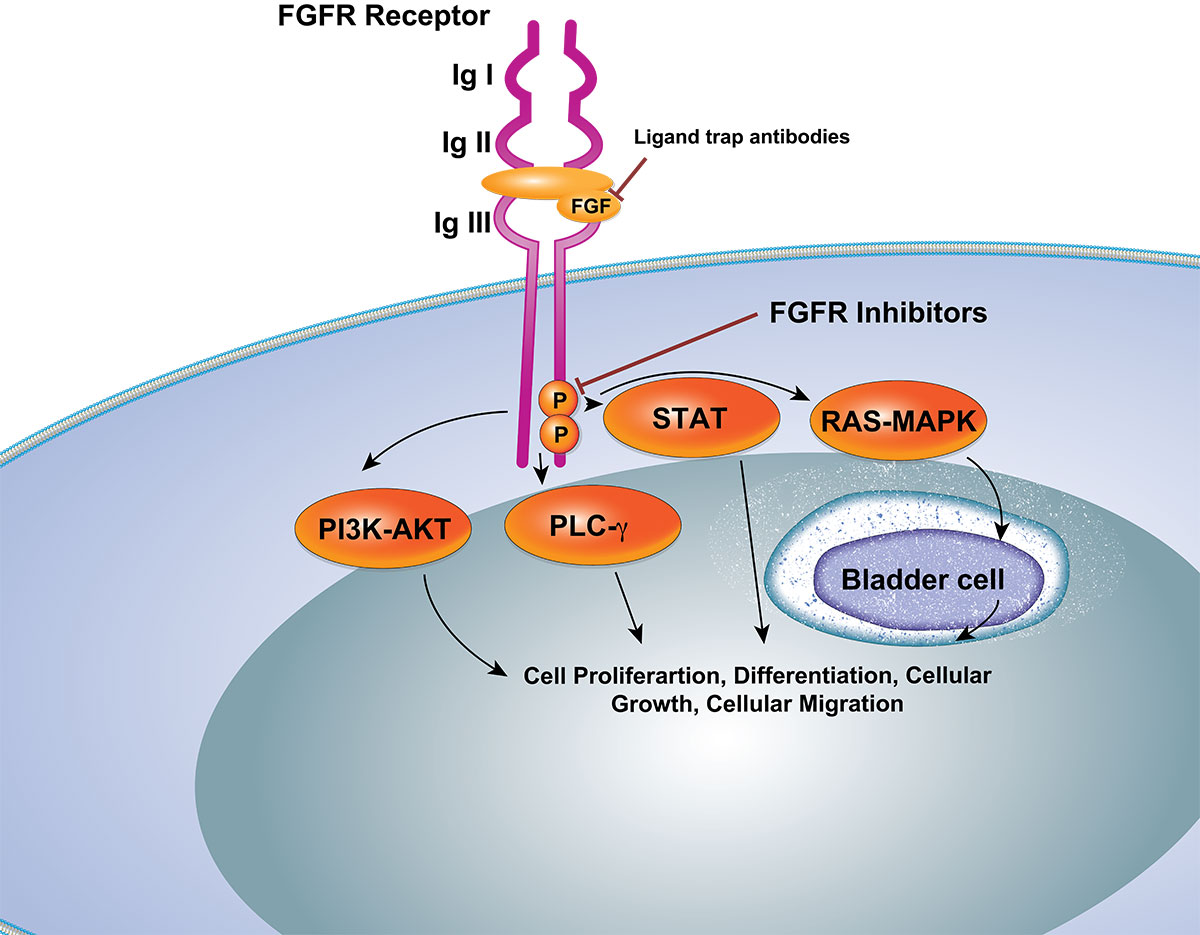
In recent years, there has been significant advancement in understanding tumor biology and the mechanisms of drug resistance in urothelial cancer. Therapeutic approaches have notably progressed with the emergence of innovative methods including immune checkpoint inhibitors and Fibroblast Growth Factor Receptor inhibitors. Nevertheless, despite the introduction of these novel agents, advanced urothelial cancer frequently continues to progress despite treatment, leading to a dismal prognosis. The advent of antibody-drug conjugates, which involve linking a target-specific monoclonal antibody to a cytotoxic agent (payload), represents a fresh and promising therapeutic strategy.
Targeting the HIF2–VEGF axis in RCC
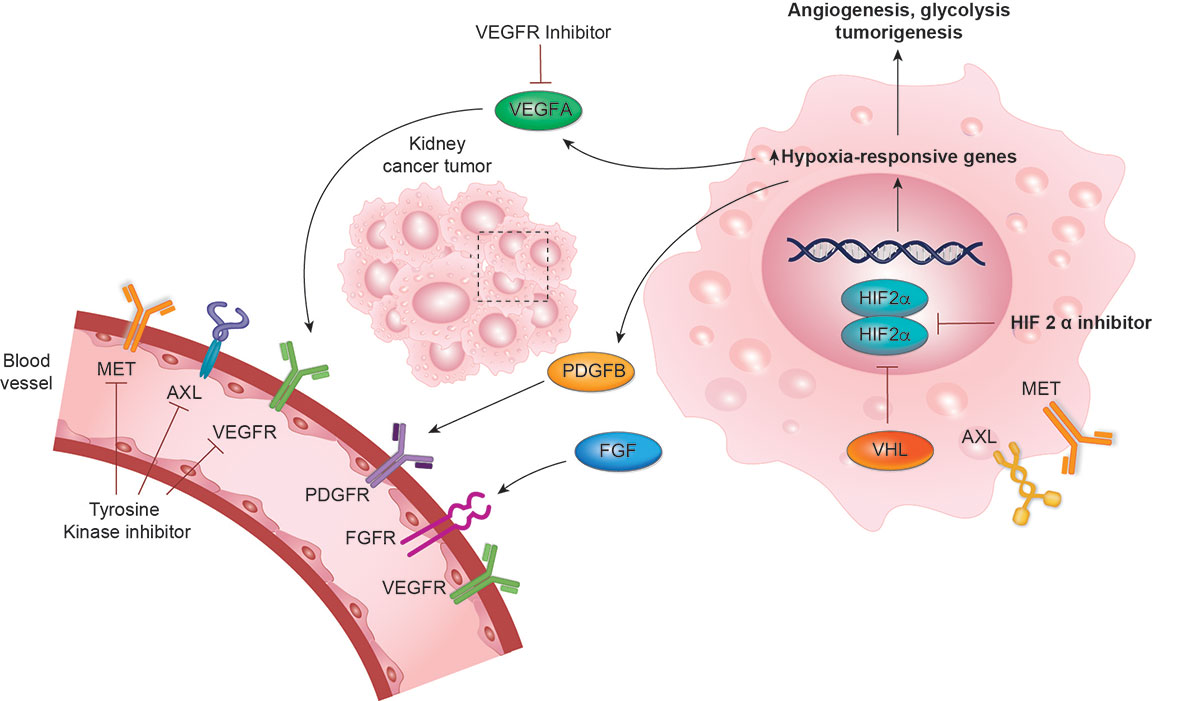
The initial treatments sanctioned for managing metastatic renal cell carcinoma (mRCC) comprised interferon-α and high-dose IL-2. Despite inducing prolonged responses in a select few patients, these medications demonstrated notably low efficacy with considerable toxicity. Consequently, they were subsequently supplanted by targeted therapeutic approaches aimed at either the endothelium of tumor vasculature (anti-VEGF drugs) or the oncogenic pathways of the tumor (mTOR inhibitors). Anti-VEGF medications encompass orally administered TKIs that target circulating VEGF or its receptors along with an intravenously administered anti-VEGF antibody. All these agents have demonstrated a progression-free survival (PFS) advantage compared to existing alternatives.
DAVA Oncology, 2700 W Plano PKWY, Plano, TX 75075, PH: 214-451-4500

